Healthcare data mapping is a crucial process that seeks to untangle the intricate web of information within the NHS. As healthcare systems increasingly rely on electronic health records (EHRs), the need for comprehensive mapping of these data flows becomes vital to ensure data transparency and effective clinical decision-making. This mapping reveals how patient information moves between providers and can illuminate gaps in data infrastructure that affect population health initiatives. By harnessing these insights, stakeholders can better understand how to utilize NHS data for improved health outcomes while adhering to privacy regulations. Furthermore, the potential of this data to drive advancements in life sciences demonstrates the value of robust healthcare data mapping in shaping the future of healthcare delivery.
The concept of healthcare data mapping can also be referred to as the systematic analysis of health information flow. This involves charting the complex pathways of electronic data generated in clinical settings, which is often stored in vast electronic health record systems. By visualizing these data transactions, it becomes possible to identify trends and issues within the healthcare ecosystem that require attention. Alternative terminology such as data infrastructure analysis and EHR flow assessment encapsulates the essence of understanding how health data is utilized across various healthcare settings. Such evaluations not only support transparency in NHS data practices but also enhance capabilities in population health management and clinical outcomes.
Understanding the Complexity of Healthcare Data Mapping
Healthcare data mapping represents a critical endeavor in understanding the intricate landscape of patient information management. As healthcare systems evolve, particularly within frameworks like the NHS, it’s essential to conduct comprehensive analyses of electronic data flows. Mapping these flows allows stakeholders to visualize how data is generated, utilized, and shared across various platforms, ensuring that essential information reaches the appropriate channels. By employing detailed methodologies, researchers can pinpoint challenges such as data fragmentation and reveal opportunities to enhance the overall data architecture, thus improving interactions between patients and providers.
This initiative not only emphasizes NHS data transparency but also seeks to strengthen data infrastructure by identifying existing gaps in the system. The key findings from such mapping exercises provide a wealth of insights into how well healthcare organizations are utilizing electronic health records (EHRs) and managing data privacy concerns. Furthermore, a clearer understanding of healthcare data flows can facilitate improved governance and accountability, enabling more informed clinical decision-making and better health outcomes.
The Role of Electronic Health Records in Population Health Management
Electronic health records (EHRs) have transformed the landscape of patient data management, serving as a robust foundation for population health initiatives. These digital records, which encompass a wide range of information—from clinical notes to diagnostic results—play a pivotal role in providing healthcare providers with real-time access to patient data. This accessibility supports timely clinical decision-making and promotes enhanced care delivery tailored to the specific needs of populations. Furthermore, by analyzing aggregated EHR data, healthcare organizations can uncover trends and disparities that inform public health strategies and policy making.
As the NHS continues to explore avenues for improving healthcare delivery, the integration of advanced data analytics with EHR systems holds great potential. An initiative focused on harnessing this big data can lead to the development of personalized medicine approaches, where tailored interventions are crafted based on comprehensive health data insights. By maximizing the value derived from EHRs, stakeholders can better understand the health trends within populations, fostering initiatives that are proactive rather than reactive in nature.
Enhancing Data Infrastructure for Improved Healthcare Outcomes
To truly capitalize on the potential of healthcare data, there needs to be a concerted effort towards modernizing existing data infrastructures. This involves investing in technologies that not only maximize data accessibility but also ensure that data integrity is maintained throughout its lifecycle. A robust data infrastructure can facilitate seamless exchanges between various stakeholders, including healthcare providers, researchers, and policymakers. Such dynamism is vital for fostering an environment conducive to evidence-based clinical decision-making that ultimately leads to improved patient outcomes.
Moreover, the need for enhanced data infrastructure is underscored by the increasing complexities posed by evolving healthcare needs and the rise of digital health solutions. A strategic focus on empowering care providers with streamlined data access and analytical tools can promote more informed public health interventions. As illustrated in the recent NHS funding allocations, investing in unified data platforms can unlock potential synergies, facilitating efficient resource allocation while ensuring that healthcare initiatives are executed effectively and transparently.
NHS Data Transparency and Its Importance
NHS data transparency is paramount in building public trust and ensuring that healthcare practices are accountable. Through initiatives like Data Insights, stakeholders can access detailed information on how patient data is generated, stored, and utilized. This level of transparency is essential for reassuring patients that their information is being handled responsibly, especially in a climate where data privacy and security are under heightened scrutiny. Transparency not only empowers patients to understand the value of their contributions to research but also educates them on their rights concerning data use.
Moreover, improved NHS data transparency facilitates enhanced collaborative efforts between healthcare providers and researchers. By making data accessible, it enables the exploration of diverse research methodologies and encourages data-driven innovations in clinical practices. As healthcare organizations strive for excellence in patient care, fostering an environment of transparency is critical to driving improvements in population health outcomes, thereby shaping the future of healthcare delivery.
Clinical Decision-Making: The Data-Driven Advantage
Incorporating comprehensive data analytics into clinical decision-making processes has become a transformative approach in modern healthcare. By leveraging big data derived from electronic health records and patient registries, clinicians can make informed choices that significantly improve patient care. The availability of detailed patient histories and population-specific health statistics enables healthcare providers to identify potential health risks early and implement appropriate interventions swiftly.
Utilizing healthcare data in decision-making presents a clear advantage in customizing treatment plans. This nuanced approach allows clinicians to consider not only individual patient needs but also broader population health trends, leading to better health outcomes. Ultimately, the integration of data-driven strategies in healthcare not only enhances operational efficiency but also ensures that the NHS can respond adeptly to the evolving needs of its population.
Addressing Data Protection and Patient Trust
As healthcare organizations increasingly harness the power of data for improving public health initiatives, data protection remains a top priority. Protecting patient information must be intertwined with any strategy aimed at enhancing healthcare delivery. The mapping exercise has brought to light existing gaps in data reporting practices, highlighting the potential for misunderstandings among patients regarding how their data is utilized. Addressing these concerns is vital to maintaining patient trust, which is foundational to successful healthcare delivery.
Healthcare organizations are tasked with transparent reporting and communication strategies that clarify data usage and the protections afforded to patient information. This includes adhering to data protection legislation to safeguard against unauthorized access or misuse of sensitive information. Increasing the transparency surrounding data practices not only fosters public confidence but also encourages patients to engage with their healthcare system fully, knowing their privacy is respected.
Optimizing Research Utilization of Healthcare Data
The effective use of healthcare data for research purposes plays a crucial role in advancing medical knowledge and improving patient care outcomes. Researchers, particularly those affiliated with universities like Imperial College London, are leveraging electronic health records and other data sources to uncover insights that inform clinical practices and health policies. By facilitating access to comprehensive datasets, the healthcare system can harness findings that contribute to evidence-based improvements and innovations.
However, for research to be beneficial, it must be underpinned by ethical standards and an understanding of data governance. Implementing protocols that ensure respectful and responsible use of healthcare data is imperative for maintaining the integrity of research activities. Also, as the NHS continues to allocate resources toward research initiatives, fostering an environment that prioritizes ethical considerations will promote collaboration and yield results that are advantageous to both healthcare providers and patients alike.
Navigating the Future of Data in Healthcare
The ongoing evolution of healthcare systems necessitates a forward-thinking approach to data management and utilization. As digital health technologies advance, the potential applications of big data in healthcare are expanding, providing unprecedented opportunities for enhancing the quality of care. With substantial financial investment targeting the development of federated data platforms, the NHS aims to ensure that patient data is leveraged effectively to inform population health strategies.
Looking ahead, the challenge will be not just to gather vast amounts of data but to cultivate an infrastructure that ensures this information is accessible and actionable. This requires collaboration across various sectors, including technology and academia, to construct cohesive frameworks that enhance clinical decision-making and prioritize patient outcomes. By championing innovative data solutions and prioritizing transparency, the NHS can pave the way for a future where healthcare data drives transformative improvements in patient care.
Frequently Asked Questions
What is healthcare data mapping and why is it important for NHS data transparency?
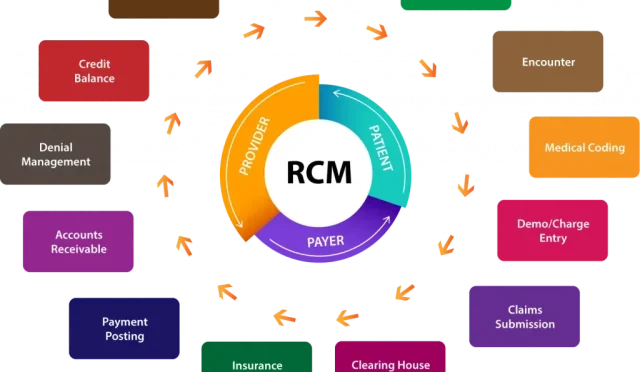
Healthcare data mapping involves the comprehensive evaluation of electronic health records (EHRs) and data flows within the NHS. This process is vital for NHS data transparency as it uncovers how data is shared among healthcare providers, identifies gaps in current practices, and informs policy objectives aimed at improving the integrity and accessibility of patient data.
How does healthcare data mapping enhance clinical decision making in the NHS?
By mapping the flow of healthcare data, including EHRs, the NHS can improve clinical decision making through better data accessibility and integration. This enables healthcare professionals to make informed decisions based on comprehensive population health data, ultimately leading to improved patient outcomes and enhanced clinical practices.
In what ways can healthcare data mapping support population health initiatives?
Healthcare data mapping can significantly benefit population health initiatives by transforming EHR data into large datasets that reveal health trends, disparities, and outcome measures. This information supports targeted public health interventions, resource allocation, and enhances the overall management of community health needs.
What role does healthcare data mapping play in the development of the NHS’s data infrastructure?
Healthcare data mapping plays a crucial role in the development of the NHS’s data infrastructure by providing a clear view of existing data assets and flows. This mapping exercise highlights areas needing improvement and informs investment decisions, facilitating a cohesive and efficient data ecosystem that enhances accessibility and interoperability across the healthcare system.
How does healthcare data mapping facilitate effective collaboration in life sciences?
Healthcare data mapping facilitates effective collaboration in life sciences by ensuring that researchers and institutions have access to comprehensive and reliable datasets derived from EHRs. This accessibility promotes well-informed research practices, enhances the quality of studies, and fosters partnerships that can drive innovation in healthcare solutions.
What are the potential risks associated with healthcare data mapping in relation to patient trust?
The potential risks associated with healthcare data mapping include concerns over data privacy and the accurate reporting of how patient data is used. If patients feel uncertain about how their EHRs are being utilized or if there are lapses in transparency, this can erode trust in the healthcare system. Robust mapping and transparent practices are essential to mitigate these risks.
What are the benefits of improving transparency in NHS data mapping?
Improving transparency in NHS data mapping provides numerous benefits, including increased patient trust, better informed healthcare decisions, and enhanced accountability in data usage. By clearly showcasing how data is generated and used within the healthcare landscape, stakeholders can ensure ethical and responsible use of patient data while fostering public confidence.
How can healthcare data mapping lead to better patient outcomes?
Healthcare data mapping can lead to better patient outcomes by providing clinicians with access to critical health information that enhances diagnostic accuracy and therapeutic effectiveness. By utilizing comprehensive datasets, healthcare providers can tailor treatments to individual patient needs, thereby improving the quality of care and reducing health disparities.
| Key Points | Details |
|---|---|
| NHS Data Mapping | A comprehensive mapping of electronic data flows within the NHS was conducted, revealing complexities in data transactions. |
| Significance of Data | The collected data can enhance clinical decision-making and support personalized medicine. |
| Transparency and Trust Issues | The mapping highlights deficiencies in how data is shared, with implications for patient transparency and data access. |
| Data Insights Platform | The platform aims to improve understanding of NHS data usage and promote transparency. |
| Focus on Ethical Use | Universities are among the primary users of NHS data for ethically approved research. |
| Investment Recommendations | Investment is encouraged to unlock inaccessible data and improve data infrastructures rather than merely reorganizing existing data. |
Summary
Healthcare data mapping is essential for understanding the intricate web of data flows within the NHS. The recent comprehensive mapping initiative has unveiled significant insights and deficiencies that challenge existing healthcare practices. By identifying gaps in transparency and data management, this research lays the groundwork for facilitating better patient trust and enhancing clinical outcomes. Investing in improved data infrastructures is crucial for realizing the transformative potential of healthcare data, ultimately leading to better healthcare services for the population.