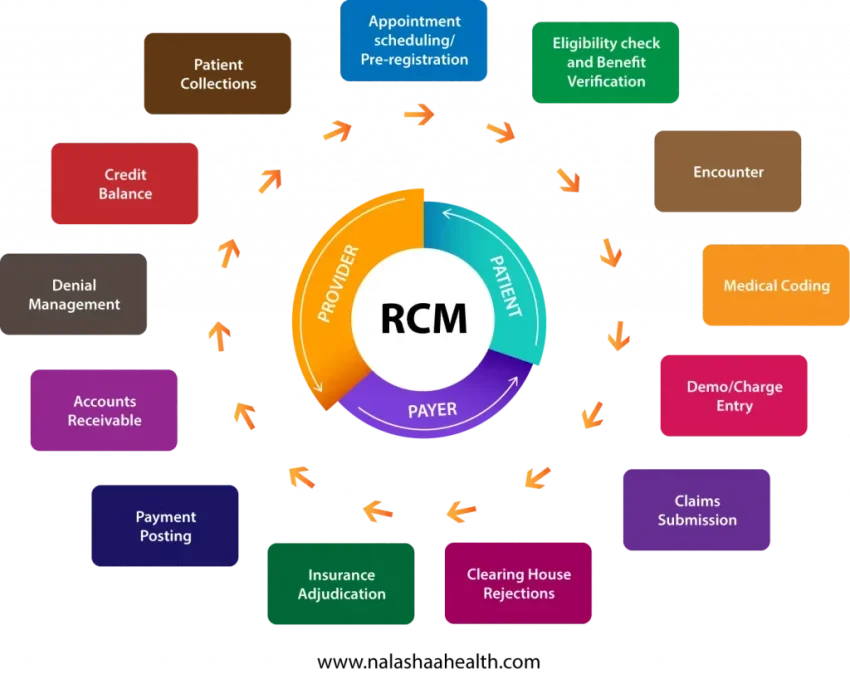
Healthcare RCM Software: Transforming Medical Billing
Healthcare RCM Software is revolutionizing the way medical facilities manage their revenue cycles and patient billing. By leveraging advanced technology, particularly AI medical billing software, these solutions not only streamline operations but also enhance patient care efficiency. Automated billing solutions are designed to simplify the complexities of healthcare revenue cycle management, enabling clinics to focus more on patient interactions rather than administrative burdens. With features like daily claim submissions and real-time tracking, billing automation for clinics has never been more effective. As the healthcare industry faces increasing demands, adopting such innovative systems is critical for maintaining optimal operational balance.
Revenue cycle management solutions within the healthcare sector are essential for optimizing financial processes and ensuring timely reimbursement. Terms like automated billing platforms and AI-driven billing systems illustrate the shift towards innovation in medical billing practices. These technologies not only enhance efficiency but also provide healthcare providers with actionable insights, leading to improved patient outcomes. By simplifying the billing process, facilities can devote more resources to direct patient care, ultimately fostering a more effective healthcare environment. In the ever-evolving landscape of healthcare administration, embracing such advancements is crucial for sustained success and operational clarity.
Understanding Healthcare RCM Software and Its Benefits
Healthcare Revenue Cycle Management (RCM) software plays a crucial role in optimizing the efficiency of medical billing processes. By leveraging advanced automation and AI technologies, these systems streamline billing operations, reduce errors, and enhance overall productivity. In a heavily regulated and complex healthcare environment, effective RCM software enables medical facilities to manage claims processing and revenue collection more effectively, ensuring that they receive timely payments and maintain financial health.
The adoption of RCM software not only improves revenue generation but also reduces the administrative burden on healthcare providers. By automating various tasks such as claim submissions and eligibility verifications, RCM software allows healthcare professionals to focus more on patient care rather than getting bogged down with intricate billing procedures. Ultimately, this leads to improved patient satisfaction and better health outcomes.
The Rise of AI Medical Billing Software
AI medical billing software has revolutionized the healthcare sector by introducing intelligent automation into billing processes. This technology utilizes machine learning algorithms to analyze data from previous claims, identifying trends and potential errors before they occur. This predictive capability ensures that billing is consistently accurate, minimizing the chances of claim denials and enhancing cash flow for healthcare facilities.
Moreover, AI solutions for medical billing drastically reduce the time and effort required for processing claims. They can automatically generate invoices based on patient visits and treatment plans, which helps to speed up the reimbursement cycle. With a quicker turnaround time for payments, healthcare providers can allocate more resources towards improving patient care and expanding their services, ultimately enhancing the overall healthcare experience.
Automated Billing Solutions for Enhanced Patient Care Efficiency
Automated billing solutions are designed to improve not only the efficiency of the revenue cycle but also to enhance the quality of patient care. By streamlining billing workflows, healthcare providers can ensure that administrative tasks don’t overshadow their primary focus on patient well-being. Automated solutions handle routine tasks, which allows staff to dedicate more time to patient interactions and care management.
Furthermore, these solutions enhance the transparency and accessibility of billing information for patients. With real-time updates on claims status and automated notifications regarding payments, patients are kept in the loop about their financial responsibilities. This openness fosters trust and satisfaction, making for a more positive overall experience within the healthcare ecosystem.
Improving Cash Flow with Automated Billing for Clinics
Cash flow is the lifeblood of any healthcare practice, and automated billing for clinics can significantly enhance it. By ensuring that claims are submitted immediately after patient visits and scheduling payments through integrated systems, clinics can minimize delays associated with manual billing processes. This swift action leads to quicker reimbursements from insurers, thereby stabilizing the clinic’s finances.
Additionally, automated billing systems come with features that help to identify and rectify potential payment issues before they escalate. This proactive approach ensures that clinics can maintain a healthy cash flow while also focusing on delivering high-quality healthcare services. The result is a seamless operation that benefits both the clinic and its patients.
The Role of Denial Prevention in Healthcare RCM
Denial prevention is a pivotal element of effective healthcare RCM software. By utilizing data analytics and sophisticated algorithms, these systems can identify potential claim denial causes upfront, enabling healthcare providers to address issues proactively. This not only decreases the number of rejected claims but also speeds up the revenue cycle, as fewer claims require re-submission.
Implementing important denial prevention strategies fosters a culture of accountability within healthcare organizations. Staff can be trained to understand common denial reasons and equipped with tools to preemptively resolve these issues. As a result, healthcare organizations can boost their efficiency and improve their overall financial health while focusing on patient care.
Leveraging Real-Time Reporting for Financial Insights
Real-time reporting is essential for healthcare organizations aiming to optimize their revenue cycles. By utilizing healthcare RCM software that offers live reporting capabilities, providers can gain immediate insights into their claims’ states, payment timelines, and revenue projections. This data-driven approach allows organizations to make informed decisions, ultimately leading to better management of financial resources and strategy development.
Moreover, the transparency provided by real-time reporting tools can enhance communication between departments. Financial and clinical teams can work collaboratively to address bottlenecks and rectify problems as they arise, ensuring that both patient care and revenue cycle management are executed seamlessly. This synthesis of functions leads to improved operational efficiency and superior patient outcomes.
The Importance of Security in Healthcare Billing Systems
As healthcare organizations increasingly transition to digital records and automated billing solutions, ensuring best-in-class security becomes paramount. Cybersecurity threats can lead to data breaches that compromise sensitive patient information, which can have severe financial and reputational consequences. Consequently, healthcare RCM software must incorporate advanced security measures, including encrypted data storage and proactive monitoring systems.
Healthcare providers must invest in robust security protocols to protect their billing systems and safeguard patient data. By prioritizing security within their RCM processes, organizations can not only comply with regulatory requirements but also build trust with their patients. This commitment to data protection is crucial for fostering strong patient-provider relationships and maintaining an organization’s integrity.
Embracing Future Innovations in Healthcare RCM
As the healthcare industry evolves, so do the technologies that support revenue cycle management. Embracing innovations such as artificial intelligence, machine learning, and comprehensive billing automation is essential for staying competitive. These advancements enhance the accuracy and efficiency of billing processes, ultimately benefiting both healthcare providers and patients.
Looking ahead, organizations should be prepared to adapt to emerging technologies that can further streamline their operations. By investing in future-proof RCM solutions, healthcare providers can ensure they are equipped to thrive in an increasingly complex landscape. Continuous enhancement of revenue cycle strategies will ultimately lead to a more sustainable and effective healthcare delivery model.
Streamlining Pediatric and Long-term Care with RCM Solutions
Pediatric care and long-term care services often present unique challenges in billing and revenue cycle management. Specialized healthcare RCM software can cater specifically to these areas, addressing the complexities of billing for diverse services such as autism therapies and elderly care. By implementing tailored solutions, providers can streamline their operations, ensuring that claims are submitted accurately and efficiently.
Additionally, utilizing RCM solutions built for pediatric and long-term care can enhance operational efficiency. Automated scheduling and billing functionalities allow healthcare providers to focus on delivering care, knowing that their billing processes are under control. This not only improves the financial viability of such services but also contributes to better patient experiences as providers can concentrate on providing support.
Frequently Asked Questions
What is Healthcare RCM Software and how does it improve billing processes?
Healthcare RCM Software, like Camber, streamlines healthcare revenue cycle management by automating billing processes, reducing denials, and enhancing cash flow. This leads to a quicker collection of payments, with many systems achieving 98% collection rates within the first 30 days.
How can AI medical billing software enhance patient care efficiency?
AI medical billing software optimizes billing automation for clinics by reducing administrative burden and minimizing errors in claims submissions. This allows healthcare providers to focus more on patient care, ultimately improving overall patient satisfaction and outcomes.
What are the benefits of using automated billing solutions in healthcare?
Automated billing solutions improve accuracy and speed in the billing process, ensure timely claim submissions, and provide real-time tracking of payments. This leads to increased efficiency in healthcare revenue cycle management and reduces the workload for administrative staff.
Can Healthcare RCM Software help in denial prevention?
Yes, Healthcare RCM Software includes features that prevent denials by identifying potential issues before they escalate. This proactive approach is crucial for maintaining cash flow and ensuring that healthcare providers receive timely payments.
What role does billing automation for clinics play in revenue cycle management?
Billing automation for clinics reduces manual processing time, minimizes human errors, and enhances reporting capabilities. Effective healthcare revenue cycle management relies on these automated processes to maintain efficient operations and financial health.
How does real-time reporting contribute to Healthcare RCM Software effectiveness?
Real-time reporting within Healthcare RCM Software provides visibility into each claim’s status, helping facilities manage their finances more effectively. This transparency allows clinics to make informed decisions and enhance revenue cycle management strategies.
What specific features should I look for in a Healthcare RCM Software?
When selecting Healthcare RCM Software, look for features such as automated claim submission, real-time tracking, denial prevention tools, multi-view reporting, and robust security measures to protect sensitive data. These features are essential for optimizing healthcare revenue cycle management.
How does Camber enhance billing automation for clinics specializing in pediatric care?
Camber’s Healthcare RCM Software offers specialized billing automation tailored for pediatric care, including autism therapy and behavioral health programs. This ensures accurate and prompt billing, allowing clinics to focus more on patient engagement and care quality.
What impact does Camber’s AI medical billing software have on cash flow for healthcare providers?
Camber’s AI medical billing software significantly accelerates cash flow by ensuring claims are submitted promptly and tracked in real-time. This reduces waiting times for payments, helping healthcare providers maintain a healthy financial status.
How can I expect my clinic to benefit from using automated billing solutions?
By implementing automated billing solutions like Camber’s, your clinic can expect reduced billing stress, increased operational efficiency, and more time to focus on patient care. This results in better patient experiences and enhanced overall service delivery.
| Feature | Description |
|---|---|
| Launch Update | Camber, previously Juniper, has launched from stealth mode. |
| Key Benefits | Focuses on healthcare administration, enabling providers to concentrate on patient care. |
| Data Intelligence | Utilizes $2B of annual therapy claims data for better billing accuracy. |
| Collection Rate | Achieves a 98% collection rate, with 93% collected within 30 days. |
| Automated Claim Submission | Automates daily claims submission and offers real-time tracking capabilities. |
| Reporting | Provides live, multi-view reporting for comprehensive insights. |
| Specialization | Tailored solutions for pediatric care, long-term care, and substance use care. |
| Denial Prevention | Identifies potential denial issues early to mitigate problems. |
| Insurance Billing | Automates claims submission once patient sessions are signed off, with tracking by various metrics. |
| Customer Testimonials | Users report transformative visibility and control over their revenue cycle. |
| Security Features | Provides robust security measures, including intrusion monitoring and firewalls. |
Summary
Healthcare RCM Software like Camber is revolutionizing the way healthcare providers manage their revenue cycle. With its powerful automated billing and real-time tracking capabilities, Camber allows clinics to focus on patient care rather than administrative tasks. The software efficiently minimizes billing stress, ensuring a high collection rate and streamlined operations. By harnessing vast amounts of therapy claims data and emphasizing denial prevention, Camber not only simplifies billing processes but also enhances financial outcomes for healthcare organizations. This makes Camber a vital partner for any healthcare facility looking to improve its revenue cycle management.
#RCMSoftware #HealthcareBilling #MedicalTech #RevenueCycleManagement #HealthcareInnovation