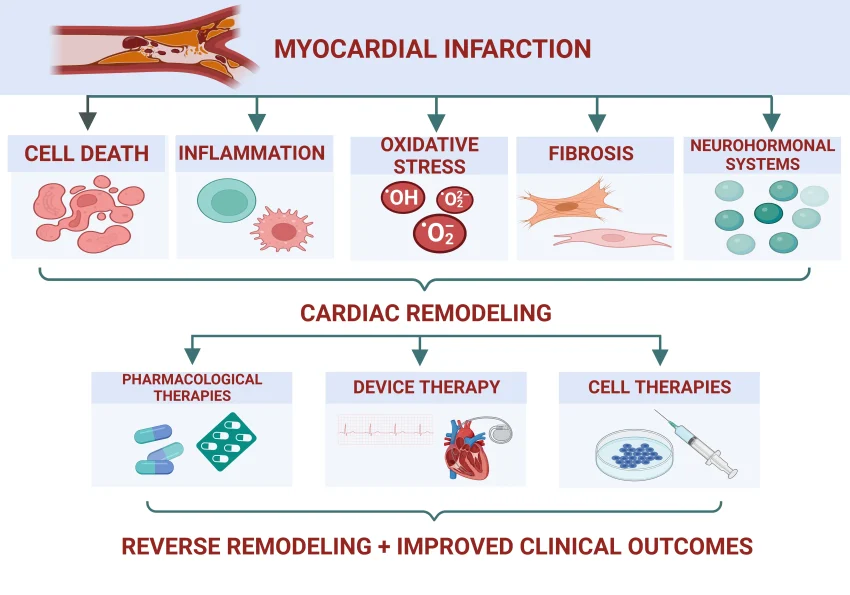
Inflammation predicts heart disease more strongly than cholesterol, reshaping how clinicians assess risk and guide prevention. The evidence highlights hs-CRP heart disease risk as a practical biomarker alongside traditional lipids. There is growing momentum for broader measurement of this inflammatory signal, with screening considered in diverse risk groups. Because clinicians treat what they measure, integrating this biomarker could reduce residual inflammatory risk beyond cholesterol alone. For those taking action, lifestyle changes and targeted approaches to dampen inflammation show promise for protecting heart health.
Viewed through an LSI-inspired lens, the topic shifts from a single marker to the wider inflammatory burden affecting the vessels. This approach uses related terms such as systemic inflammation and vascular inflammation to describe risk without relying on a single test. Inflammatory biomarkers and immune-driven processes inform risk stratification and personalized prevention strategies. Trials continue to explore anti-inflammatory therapies for heart disease and their role alongside statins and lifestyle changes. By connecting traditional risk factors with broader inflammatory concepts, clinicians can communicate clearer guidance and optimize care.
Inflammation predicts heart disease: A Stronger Predictor Than Cholesterol
New ACC recommendations place inflammation at the center of risk assessment by endorsing hs-CRP blood testing. Inflammation, as measured by hs-CRP, now appears to predict heart disease more reliably than cholesterol alone, reshaping our view of hs-CRP heart disease risk. This shift reinforces inflammation biomarkers heart health and supports a broader framework of inflammation and cardiovascular risk beyond lipid levels.
Reducing inflammation is not a placebo effect; statins lower hs-CRP levels and can reduce events, yet inflammatory risk persists even when LDL is well controlled. The ACC emphasizes universal hs-CRP screening to detect this residual risk, particularly in patients who may be considered low traditional risk yet have high inflammation. This approach aligns with the idea of anti-inflammatory therapies heart disease offered as a targeted way to lower overall risk.
Universal hs-CRP Screening and Cardiovascular Risk Assessment
Universal hs-CRP screening is now recommended for both primary and secondary prevention, integrating inflammatory status into cardiovascular risk stratification. Measuring hs-CRP adds a layer of information beyond cholesterol, helping clinicians assess inflammation and cardiovascular risk when LDL is not the whole story.
For patients, a hs-CRP result can guide decisions about lifestyle changes, statin therapy, and consideration of anti-inflammatory strategies. When used alongside lipid panels, hepatic and kidney function tests, and blood pressure data, this approach supports a comprehensive view of inflammation biomarkers heart health and risk reduction.
Inflammation Biomarkers Heart Health Beyond LDL
While LDL cholesterol remains a key factor, other inflammation biomarkers provide complementary signals. Markers such as IL-6, fibrinogen, and neutrophil-to-lymphocyte ratio have been studied, but once hs-CRP is known, additional signals offer diminishing returns for routine risk assessment.
Imaging biomarkers and vascular inflammation tests show promise for niche cases but are not yet ready for routine use. The core message is that inflammation biomarkers heart health can be captured effectively with hs-CRP testing, reinforcing the idea that inflammation and cardiovascular risk are tightly linked.
What Works to Lower Inflammation: Evidence from Trials
Statins, particularly in people with elevated hs-CRP, substantially reduce inflammation and lower event rates even when LDL is normal, as highlighted by major trials like JUPITER. Anti-inflammatory therapies heart disease beyond statins have shown potential in selected populations, though benefits vary by drug and patient risk profile.
Colchicine and targeted anti-inflammatory strategies have demonstrated recurrent-event reductions in patients with established disease, supporting a role for inflammation control in prevention. Lifestyle changes, such as anti-inflammatory diets, regular exercise, smoking cessation, and weight management, also contribute to lower inflammation and fewer cardiovascular events.
Anti-inflammatory Therapies Heart Disease: What the Trials Tell Us
Clinical trials have teased apart which therapies help and which do not. Trials of methotrexate, TNF inhibitors, and corticosteroids largely failed to reduce cardiovascular events, illustrating the complexity of modulating inflammation in heart disease.
In contrast, targeted therapies like canakinumab reduced major adverse events in high-risk patients with elevated inflammation, while the cost and infection risk remain concerns. Colchicine has emerged as an accessible option for secondary prevention, highlighting the potential of anti-inflammatory therapies heart disease when properly selected.
Statin Therapy: Reducing Inflammation and Risk Even with Normal LDL
Statins do more than lower LDL; the JUPITER trial showed significant reductions in cardiovascular events in people with hs-CRP elevations despite normal LDL levels, underscoring the synergy between lipid lowering and inflammation reduction.
Even when cholesterol is controlled, lowering hs-CRP contributes to risk reduction, reinforcing inflammation and cardiovascular risk as a combined target. Healthcare providers may consider hs-CRP testing to identify patients who could benefit from statin therapy for anti-inflammatory purposes.
Colchicine in Secondary Prevention: Reducing Recurrent Events
Large trials such as COLCOT and LoDoCo2 found that low-dose colchicine reduces recurrent cardiovascular events in patients with established disease, supporting a role for anti-inflammatory therapies heart disease in secondary prevention.
Colchicine is generally well-tolerated but requires caution in kidney or liver disease, and ongoing studies continue to refine its use in primary prevention and broader populations.
Understanding hs-CRP Levels: What Counts as Risky
A simple grading system helps translate hs-CRP values into risk categories: below 1 mg/L is low risk, above 3 mg/L is high risk, with an intermediate range in between. This framework supports the ACC’s push for integrating inflammation into risk assessment.
Interpreting hs-CRP must consider comorbid conditions, age, and medication use. In the context of universal hs-CRP screening and overall inflammation and cardiovascular risk, clinicians can tailor strategies to address residual risk.
Measuring Inflammation: Practical Steps for Clinicians and Patients
hs-CRP testing is widely available and inexpensive, making it feasible to add inflammation screening to routine care. The ACC’s guidance promotes measuring hs-CRP as part of comprehensive risk assessment for people at risk and those with established disease.
Patients can discuss hs-CRP levels with their clinicians and consider next steps, including lifestyle changes and potential anti-inflammatory therapies heart disease, depending on the score and overall risk.
Lifestyle Interventions to Lower Inflammation and Heart Risk
Anti-inflammatory dietary patterns such as the Mediterranean and DASH diets, combined with regular exercise and weight management, consistently lower hs-CRP and inflammation markers while improving other heart-health metrics.
Smoking cessation, adequate sleep, and stress management further reduce inflammation and cardiovascular risk, aligning lifestyle changes with the ACC’s recommendations for universal inflammation screening and subsequent risk reduction.
Future Directions: IL-6 Inhibitors, Bempedoic Acid, and Emerging Therapies
Emerging therapies targeting IL-6 pathways and other inflammatory mechanisms are under study, with some showing promise for reducing residual inflammatory risk beyond statins.
In addition, drugs like bempedoic acid lower LDL and have early signals for lowering hs-CRP, while ongoing trials continue to test long-term outcomes and safety in relation to universal hs-CRP screening and established inflammation risk.
Conclusion: A New Era in Heart Disease Risk Management
The recognition that inflammation predicts heart disease reshapes practice by elevating hs-CRP testing and integrating anti-inflammatory strategies with cholesterol management.
As evidence accumulates from trials and guidelines, clinicians can address inflammation and cardiovascular risk in tandem—using hs-CRP to guide therapy, promoting healthy lifestyle changes, and considering targeted anti-inflammatory therapies when appropriate.
Frequently Asked Questions
Inflammation predicts heart disease: How does hs-CRP relate to risk?
hs-CRP is a simple blood marker of systemic inflammation. Higher hs-CRP levels predict heart attacks, strokes, and other cardiovascular events, sometimes even when LDL cholesterol is controlled. The ACC recommends measuring inflammation with hs-CRP as part of risk assessment because clinicians are more likely to act when risk factors are measured. If your hs-CRP is elevated, discuss strategies to reduce inflammation, including statins, lifestyle changes, and, in some cases, anti-inflammatory therapies.
Inflammation and cardiovascular risk: what is the role of universal hs-CRP screening?
Universal hs-CRP screening, as discussed in ACC guidance, helps identify residual inflammatory risk across primary and secondary prevention populations. It provides additional context beyond cholesterol levels to guide management.
Inflammation biomarkers heart health: what are key markers beyond hs-CRP?
Beyond hs-CRP, inflammation biomarkers like IL-6, fibrinogen, and neutrophil-to-lymphocyte ratio can signal cardiovascular risk, but hs-CRP remains one of the strongest signals. In many cases, measuring hs-CRP gives the clearest read on inflammation-related risk. Some clinicians may consider additional markers if results would change management, but the signal from hs-CRP is typically primary.
Anti-inflammatory therapies heart disease: Which therapies have shown benefit?
Colchicine has shown benefit in reducing recurrent cardiovascular events in people with established heart disease (COLCOT and LoDoCo2). Canakinumab reduced events in certain high-risk groups but is expensive and can increase infection risk. Other anti-inflammatory approaches such as methotrexate or TNF inhibitors have not shown clear benefits in major heart-disease trials. Lifestyle changes and proven therapies like statins remain foundational.
Inflammation predicts heart disease: How does it compare to cholesterol in risk prediction?
In some populations, hs-CRP can predict risk more strongly than LDL cholesterol, highlighting the role of inflammation in heart disease. Even with well-controlled cholesterol, a high inflammatory signal leaves residual risk. This supports treating inflammation as a distinct risk factor alongside traditional cholesterol and blood-pressure targets.
How can I lower inflammation to reduce inflammation predicts heart disease risk?
Lowering inflammation to reduce inflammation-predicts heart disease risk can be achieved with statins, which lower hs-CRP in addition to cholesterol reduction. Lifestyle strategies—anti-inflammatory diets (Mediterranean, DASH), regular exercise, weight management, and smoking cessation—also lower hs-CRP and risk. Some anti-inflammatory drugs have not proven benefits for heart disease, so work with a clinician to choose proven approaches.
Is universal hs-CRP screening recommended for everyone to assess inflammation predicts heart disease risk?
Not for everyone; guidelines favor testing in those at risk or with established disease, with decisions tailored to the patient. Discuss with your clinician whether hs-CRP testing fits your risk profile and care plan.
How should inflammation be measured when assessing inflammation predicts heart disease risk?
Use a blood hs-CRP test, which is widely available and inexpensive. Target hs-CRP levels are typically below 1 mg/L for low risk; above 3 mg/L indicates higher risk. Re-testing may be advised to track changes over time, particularly when starting therapy.
What does a high hs-CRP mean for inflammation predicts heart disease risk, and what steps to take?
A high hs-CRP indicates elevated inflammatory risk and a higher likelihood of cardiovascular events, but it is one piece of the overall risk picture. Work with a clinician to evaluate lifestyle, blood pressure, glucose, and lipid management alongside inflammation. Interventions like statins or anti-inflammatory therapies can be considered based on the entire risk profile.
What anti-inflammatory strategies do not work for inflammation predicts heart disease?
Some anti-inflammatory strategies, such as methotrexate, TNF inhibitors, and corticosteroids, have not shown cardiovascular benefits in major trials. Focus on evidence-based approaches: statins, colchicine for certain patients, and lifestyle changes to reduce inflammation. Always discuss risks and benefits with a clinician.
Are imaging biomarkers part of inflammation predicts heart disease risk assessment?
Imaging biomarkers (CT, PET, MRI) can detect vascular inflammation and may help in research settings, but they are not routine for standard heart-disease risk assessment. These tools are not yet recommended for universal screening in typical clinical practice. Routine hs-CRP testing remains the practical approach.
What is residual inflammatory risk and how is it addressed in inflammation predicts heart disease?
Residual inflammatory risk refers to ongoing inflammation despite controlled cholesterol and blood pressure. Address it with a combination of proven therapies (such as statins, where appropriate), lifestyle changes, and in selected cases anti-inflammatory strategies guided by a clinician. Universal hs-CRP screening can help identify people who might have this residual risk.
| Key Point | Summary |
|---|---|
| Inflammation (hs-CRP) is a stronger predictor of heart disease than cholesterol (LDL/ApoB). | hs-CRP provides superior risk prediction, especially when cholesterol is well-managed or in SMuRF‑less patients. |
| ACC recommends universal hs-CRP testing for primary and secondary prevention. | Testing via blood tests and counting with cholesterol informs risk assessment and management opportunities. |
| Residual inflammatory risk persists even when cholesterol is controlled. | Inflammation can drive events despite well-controlled cholesterol; non-SMuRFs are important risk sources. |
| Evidence-based strategies to lower inflammation and risk. | Statins, colchicine, and lifestyle changes reduce hs-CRP and cardiovascular events; canakinumab lowers events but with cost and infection risk. |
| What doesn’t work in trials. | Methotrexate, TNF inhibitors, and corticosteroids have not improved cardiovascular outcomes in major trials. |
| Measuring and interpreting hs-CRP. | hs-CRP testing is simple and inexpensive; target 3 mg/L is high risk; use results to guide prevention. |
Summary
Inflammation predicts heart disease more strongly than cholesterol, and new ACC guidance urges universal hs-CRP testing for primary and secondary prevention. This shift underscores inflammation as a modifiable risk factor alongside traditional cholesterol measures. Evidence from trials supports reducing hs-CRP and cardiovascular events with statins, colchicine, and lifestyle changes, while some anti-inflammatory drugs have not yielded benefits. Measuring hs-CRP is simple and inexpensive, enabling doctors and patients to address residual inflammatory risk even when cholesterol appears controlled. By prioritizing inflammation assessment in routine care, individuals can take proactive steps—through medication choices, diet, exercise, and smoking cessation—to lower heart disease risk.