Pharmacy Benefit Management (PBM) plays a crucial role in today’s healthcare landscape, streamlining the delivery of medication and ensuring affordable access to prescription drugs. As a vital component of Health Benefit Management, PBMs not only negotiate prices but also enhance patient care by managing pharmacy benefits effectively. With the rise of innovative Pharmacy Management Solutions, organizations can now leverage technology to improve their medical benefit administration processes. From AI-powered health platforms that provide insights into medication usage to Transparent PBM Solutions that promise clarity in pricing, the industry is evolving rapidly. By prioritizing affordability and accessibility, Pharmacy Benefit Management is set to transform the way patients receive their medications and manage their health.
When discussing the intricacies of managing prescription drug benefits, terms such as Rx Benefits Administration and pharmacy management come to the forefront. These systems are designed to optimize the management of healthcare perks, ensuring that clients—whether they are employers, health plans, or members—receive maximum value. By employing advanced technologies, like AI-driven frameworks and thorough benefit oversight, organizations can develop more efficient medical benefit strategies. This approach enables a better alignment of health services, fostering an environment where patients can access medications with greater ease and transparency. In an era where healthcare costs continue to rise, finding effective solutions in pharmacy benefit management is paramount to delivering quality care.
Understanding Pharmacy Benefit Management
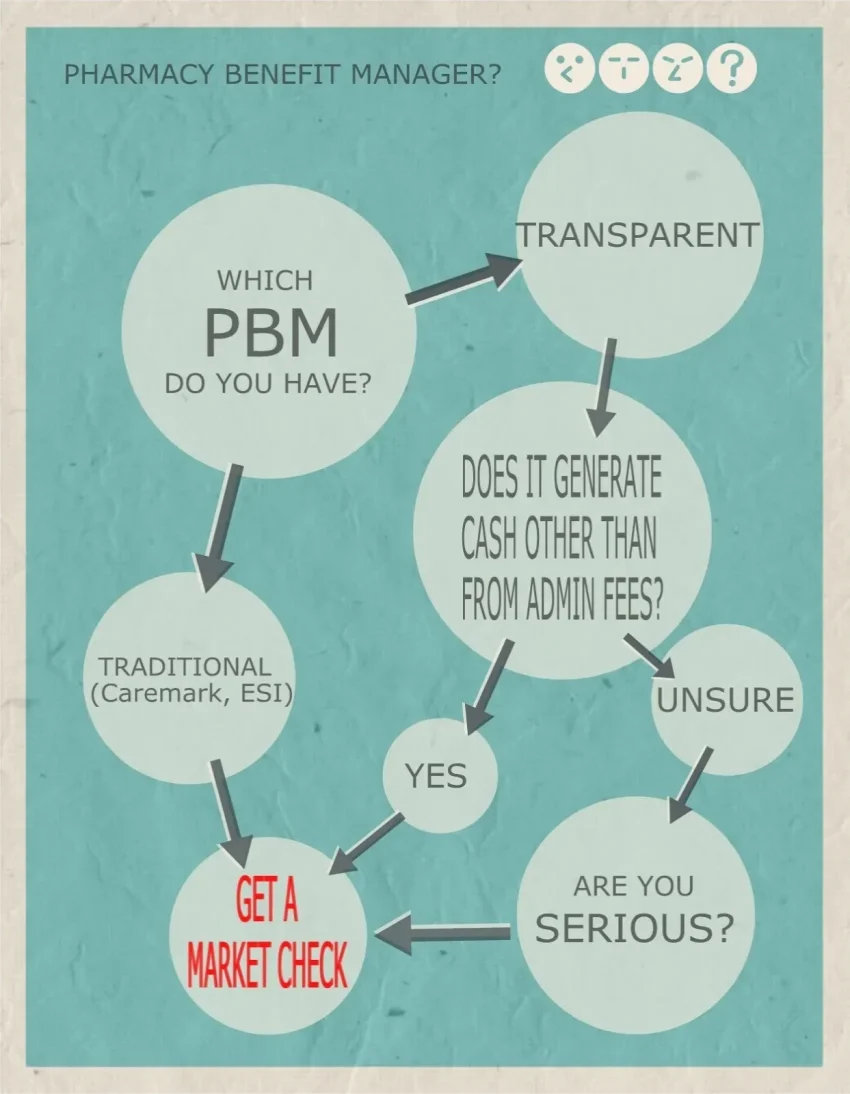
Pharmacy Benefit Management (PBM) is a crucial component of managing prescription drug benefits for health plans and employers. PBMs serve as intermediaries between insurers, pharmacies, and pharmaceutical manufacturers, streamlining the management of medication benefits. This involves negotiating discounts with drug manufacturers, managing formularies, and processing claims. An effective PBM reduces healthcare costs while maintaining high standards of care by ensuring that members have access to necessary medications at an affordable price.
In recent years, there has been a growing emphasis on transparent PBM solutions to foster trust and accountability in healthcare. Providers and employers increasingly prefer models that offer clear insights into pricing and rebates. By embracing transparent pharmacy benefit management practices, companies can align their strategies with the ongoing push for affordability and comprehensive patient care, ultimately resulting in better health outcomes and financial sustainability.
Benefits of Unified Pharmacy and Medical Benefit Management
Unified Pharmacy and Medical Benefit Management provides a holistic approach to healthcare administration, allowing both medical and pharmacy services to be integrated under one roof. This integration helps streamline processes for employers and health plans, reducing administrative burdens while enhancing efficiency. Such a model facilitates better communication and coordination of care between healthcare providers, ultimately improving the patient experience by minimizing disruptions and ensuring seamless access to needed services.
Moreover, integrated benefit management solutions leverage technology to provide real-time data and analytics, empowering stakeholders in the healthcare system. With AI-powered health platforms, like those offered by Judi Health, organizations can better predict trends, adjust care management programs, and closely monitor patient health outcomes. This level of comprehensive management is essential not just for cost efficiency but for driving innovation in the healthcare space.
As organizations continue to look for ways to optimize their healthcare spending, the shift towards unified benefit management is becoming increasingly desirable. By moving away from fragmented services, healthcare stakeholders can deliver coordinated care that ultimately benefits both patients and payers alike.
The Role of AI in Health Benefit Administration
AI-powered health platforms are transforming the landscape of healthcare by streamlining processes such as claims management and patient navigation. Through the implementation of data analytics and machine learning, organizations can enhance their operational efficiency and better predict patient needs. Tools like those offered in the unified health benefit administration enable health plans and employers to make data-driven decisions, thus improving overall service delivery and satisfaction among members.
Furthermore, leveraging artificial intelligence in health benefit administration allows for a more personalized approach to care. By analyzing large sets of patient data, AI can identify trends and tailor care plans that cater to individual health needs. This not only optimizes therapeutic outcomes but also fosters a proactive rather than reactive healthcare approach, ultimately leading to healthier communities and lower overall healthcare costs.
Transforming Health Benefits with Digital Solutions
The integration of digital solutions is pivotal for modernizing health benefit management. Organizations like Judi Health are leveraging next-generation technologies to enhance both pharmacy and medical benefit administration solutions. This transformation is crucial in improving access to insights and resources for various stakeholders, including employers, brokers, and health plan members. By utilizing these innovative tools, healthcare providers can offer more effective services, accommodating the diverse needs of their members.
Additionally, digital platforms enhance communication between providers and patients. With user-friendly interfaces, members can easily access their health benefit information, schedule appointments, and communicate with healthcare providers. This shift not only optimizes the administrative workflow but also enhances patient engagement and empowerment, vital components for achieving better health outcomes in the long run.
The Importance of Transparency in Pharmacy Management Solutions
Transparency in pharmacy management solutions is critical for building trust between all stakeholders involved in healthcare. Employers, health plan members, and providers benefit when organizations are open about pricing structures, drug formularies, and rebate arrangements. Companies such as Capital Rx are spearheading these efforts by implementing clear, transparent practices that demystify the complexities of pharmaceutical pricing and benefits, enabling informed decision-making across the board.
Moreover, transparent pharmacy benefit management allows employers to understand and control their healthcare costs better. With clear insights into drug pricing and utilization, organizations can identify opportunities for savings and make strategic adjustments to their health plans. This commitment to transparency not only supports cost containment efforts but also elevates the importance of quality patient care by ensuring access to necessary medications without burdensome hidden fees.
Navigating the Evolving Landscape of Health Benefit Management
The landscape of health benefit management is continually evolving due to changes in regulations, advances in technology, and shifting consumer expectations. Organizations must navigate these transformations carefully to remain competitive and deliver effective health solutions. By staying informed about emerging trends and adopting innovative strategies, employers can better serve their employees and adapt to the changing healthcare environment.
Additionally, engaging with technology like AI and unified administrative platforms can significantly simplify the navigation of these complexities. Health plans can leverage data analytics to anticipate changes in benefit requirements while simultaneously enhancing member experiences. This agility not only prepares organizations for future changes but also positions them as leaders in a rapidly advancing digital healthcare ecosystem.
Empowering Brokers and Consultants in Health Benefit Delivery
Brokers and consultants play a pivotal role in the delivery of health benefits, acting as intermediaries between employers and health plans. Empowering these professionals through technology and resources can significantly enhance the value they provide to their clients. By equipping brokers with tools that offer comprehensive insights into health benefits, organizations can facilitate more informed decision-making and tailored recommendations for their clients.
Furthermore, providing education and access to transparent pharmacy benefit management solutions is essential. Brokers equipped with the right knowledge can help employers navigate complex health plans, ensuring they select the best options that meet their specific needs. This collaboration ultimately drives better outcomes, aligning with the collective goal of enhancing employee well-being and optimizing healthcare expenditures.
The Future of Pharmacy Benefits in Healthcare
As the healthcare industry continues to evolve, the future of pharmacy benefits will likely be shaped by technological advancements and the demand for transparency in health benefit management. Emerging trends indicate a shift towards personalized medicine and value-based care models, where patients receive treatments tailored to their unique health profiles. This evolving landscape necessitates innovative pharmacy management solutions that can adapt and respond to these new demands.
Additionally, the integration of artificial intelligence and big data analytics will further transform how pharmacy benefits are delivered. By leveraging advanced technologies, organizations can optimize medication management practices, resulting in better adherence rates and improved health outcomes. The future of pharmacy benefits will largely hinge on the ability of stakeholders to embrace these technologies and commit to delivering higher value care.
Building Trust through Transparent Pharmacy Benefit Management
Building trust among stakeholders in healthcare is paramount, particularly regarding pharmacy benefit management. Transparent practices foster confidence among employers, members, and healthcare providers. Organizations committed to transparency can eliminate misconceptions about pricing and benefits, enabling stakeholders to make informed choices. By openly sharing information about formularies, pricing, and drug rebates, companies can cultivate a culture of trust that benefits all parties involved.
Moreover, cultivating trust is essential in ensuring the success of health benefit management programs. When members feel confident in their health plans, they are more likely to engage with their benefits and adhere to prescribed medications. This engagement leads to improved health outcomes and, in turn, helps employers and health plans manage costs more effectively. As the industry moves toward transparency as a best practice, those who prioritize open communication will lead the way in building stronger, more trusting relationships.
Frequently Asked Questions
What is Pharmacy Benefit Management and how does it impact healthcare costs?
Pharmacy Benefit Management (PBM) involves the administration of prescription drug benefits for health plans. It plays a significant role in controlling drug costs and improving access to medications for patients. By negotiating with drug manufacturers and pharmacies, PBMs help reduce out-of-pocket expenses for members while ensuring that necessary medications are available.
How do transparent PBM solutions enhance employer health benefits?
Transparent Pharmacy Benefit Management solutions provide employers with clear insight into drug pricing, rebates, and formulary design. This transparency allows employers to understand cost drivers and make informed decisions that can lead to improved healthcare outcomes for their employees while reducing overall healthcare spending.
What services do full-service pharmacy benefit management companies offer?
Full-service pharmacy benefit management companies like Capital Rx provide a comprehensive range of services including formulary management, claims processing, and member support. These services ensure patients receive their medications promptly and at the best prices, aligning with the overall goals of health benefit management.
How can employers benefit from level-funded pharmacy benefit management?
Level-funded pharmacy benefit management allows employers to budget more effectively for their pharmacy costs. It combines the predictability of a fully-insured plan with potential savings from self-funding, thus providing a balanced approach for managing pharmacy benefits while allowing flexibility in spending based on actual usage.
What are the advantages of AI-powered health platforms in managing pharmacy benefits?
AI-powered health platforms enhance Pharmacy Benefit Management by leveraging data analytics to optimize prescription drug utilization and patient outcomes. This technology improves decision-making processes and facilitates more personalized medication management, ultimately leading to better health results for members.
How does medical benefit administration work alongside Pharmacy Benefit Management?
Medical Benefit Administration works in conjunction with Pharmacy Benefit Management to ensure comprehensive coverage for both medical and prescription services. Together, they create a seamless experience for members, enabling coordinated care that can lead to improved health outcomes and reduced costs for both patients and employers.
What should employers consider when choosing a pharmacy management solution?
When selecting a pharmacy management solution, employers should evaluate transparency in pricing, the flexibility of the program, customer service offerings, and the effectiveness of the integrated health solutions provided. Choosing a solution that aligns with their specific health benefit management needs ensures better outcomes for both the employer and its employees.
What role do brokers and consultants play in Pharmacy Benefit Management?
Brokers and consultants act as intermediaries between employers and Pharmacy Benefit Management companies. They help businesses navigate the complexities of health benefits, ensuring that they obtain the best possible pharmacy plans that meet their unique employee needs while maximizing cost effectiveness.
How do unbundled pharmacy benefit management solutions differ from traditional models?
Unbundled Pharmacy Benefit Management solutions separate the management of pharmacy benefits from other healthcare services, offering employers more customization. This flexibility allows employers to tailor services to their specific needs, potentially leading to enhanced cost control and better alignment with employee health needs.
| Feature | Description |
|---|---|
| Judi Health | Full-service health benefit management offering a range of solutions. |
| Capital Rx | Full-service pharmacy benefit management focused on affordability and transparency. |
| Judi Care | Pharmacy and medical care navigation to assist members in accessing healthcare resources. |
| Never Move Again | Unbundled pharmacy benefit management for flexible healthcare solutions. |
| Capital Equilibrium | Level-funded pharmacy benefit management to help control costs while delivering benefits. |
| Capital Rx Advantage | White-labeled discount card to provide additional savings on prescriptions. |
| Technology | AI-powered enterprise health platform designed to streamline health benefits management. |
Summary
Pharmacy Benefit Management is essential for optimizing the costs and access to medications for patients and healthcare systems. Companies like Judi Health and Capital Rx offer comprehensive solutions aimed at enhancing the management of pharmacy and medical benefits, promoting transparency, and ensuring affordability. Their innovative tools and advanced technology ensure that employees and members receive the best possible support in navigating their health plan options. With a strong focus on delivering superior health outcomes, Pharmacy Benefit Management emerges as a crucial element in the healthcare landscape.